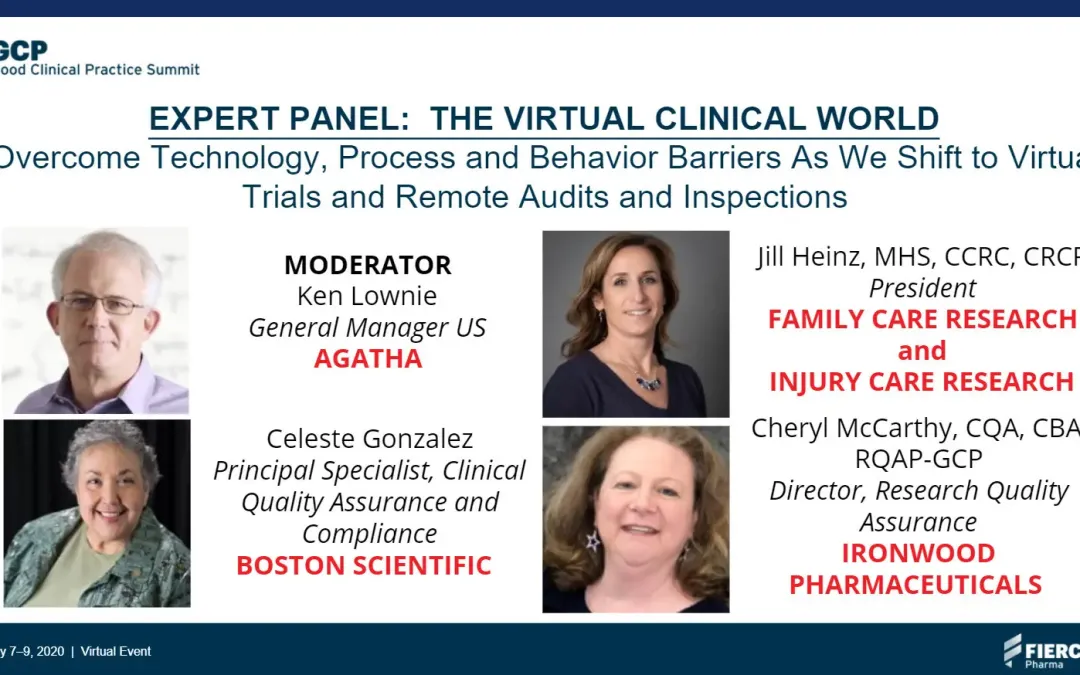
Clinical trials are facing an increasing need to go virtual, and with that change comes opportunity and challenge. At the GCP Summit earlier this month, Agatha’s Head of North American Operations, Ken Lownie, hosted a panel of clinical trial experts to get their views on the virtual clinical world. Here’s a summary of their insights.
The Shift to Remote Monitoring for Clinical Trial Sites
Jill Heinz, President of Family Care Research and Injury Care Research, pointed out that there weren’t a lot of Clinical Trial sites following a remote model pre-COVID-19. Heinz said that her companies (which are research sites) have been capable of working remotely for years, but sponsors and CROs didn’t want to work that way.
Since COVID-19, remote monitoring has been the norm. She said that there had been some requests to review on-site, but Sites are denying on-site access to CRAs (clinical research associates). Whether a Site can support remote monitoring is a different question. Heinz said it’s more difficult for sites that don’t have full electronic capabilities, but it’s the sponsors and CROs that are slowing remote monitoring down.
Celeste Gonzalez, Principal Scientist, Clinical Quality Assurance and Compliance at Boston Scientific, said that remote monitoring is a double-edged sword. She said there are regions where it’s possible, but in the EU, it’s been impossible due to GDPR compliance regulations.
Gonzalez said that COVID-19 has caused a shift in monitoring. Sites that have e-records have embraced it, but those with a hybrid model – a combination of electronic and paper records – have found it difficult. Remote monitoring goes hand-in-hand with centralized monitoring, and monitors were targeted in their approach at Sites, she said.
As Sites open back up to on-site reviews, it’s yet to be seen if monitors will be back on site. Gonzalez said that she hears remote monitoring will continue simply due to cost savings.
Cheryl McCarthy, Director, Research Quality Assurance for Ironwood Pharmaceuticals, pointed to similarities with early adopters of eCapture technology (something that has been a struggle for the industry to adopt). She said there is an opportunity to leverage technology and train people. It’s an immediate challenge, she pointed out, because things are shifting quickly. However, the shift to remote monitoring will not take the same amount of time it took for people to adopt electronic capture technology.
Obstacles to Remote Monitoring
McCarthy said that one major obstacle is regulatory. What is the FDA’s position? There hasn’t been a lot of guidance on remote monitoring and how to do certain things remotely. However, she acknowledged that the FDA’s perspective would take time as it tested some remote monitoring and found some challenges. It’s a learning process, McCarthy said, that crosses sponsors, regulatory agencies, and sites.
There is nothing in the guidelines that prevent remote monitoring, Gonzalez said. As long as there are a defined plan and risk assessment showing the agency how they went about reaching their decision to implement remote monitoring, they should be fine.
On the behavioral side, the question is, are Site Administrators ready for it? Heinz said it comes down to adoption. A lot of sites are just now getting into CTMS software, with many still have paper processed for monitoring. She pointed out that remote monitoring with paper sources is time-consuming and costly (there’s no efficient way to do it).
Hospitals have EMR (electronic medical records), so they are in a somewhat better position. However, EMR software wasn’t designed for research – they can’t give access to only individual records.
On the independent Site side, it’s less of a challenge because it’s easier to pivot and figure out the best way to support remote monitoring, Heinz said.
McCarthy said it’s about getting access to patient records. She started out working for an EMR company and has found that many sponsors still aren’t using them. EMRs are proprietary systems that require a lot of training. Then you have the privacy considerations such as HIPAA and GDPR and have to think about things from a redaction standpoint. She said that there needs to be a general understanding of how everyone can work together – that requires guidance from regulators.
The Technical Aspects of Remote Monitoring
From a technology perspective, there is still some work to be done to support remote monitoring. Do you give direct access to EMR systems? Or do you download the required documents and place them in a secure file share, redacting as necessary? McCarthy said that the basic technology is still a challenge (even things like using Zoom).
Gonzalez said that in terms of monitoring and auditing, the days are coming to an end where clinics upload paper documents into an ETMF. We are moving to eSignatures that enable the sponsors and sites to see the same document in real-time, and don’t require the monitor to see it again physically.
In terms of EMR – many things still aren’t electronic and need to be uploaded to the EMR. One challenge here is when you are dealing with certified copies and the ‘wholeness’ of that copy. This needs to be looked at from a risk perspective because if the whole document isn’t there, you don’t know what you’re missing.
Gonzalez said that she’s seeing the US moving more to an electronic system, but in the EU, there is still a long way to go.
From Heinz’s perspective, her companies have remote monitoring capabilities. They are a smaller Site, and they bought a program for eSource/Regulatory CTMS. Now that they are all set up and fully electronic, they can quickly give CRAs access that is read-only and redacted. But she knows other Sites who have to go through an IT process to provide a CRA access, and it can take days to weeks to make that happen.
If they do need to scan in something that is paper (like an EKG tracing), they still require a certified copy that is certified by the person scanning it with an electronic signature, that the document is true, accurate, and whole. With regulatory documents, they also give an in-house CRA access to ensure everything is correct.
The Cost-Benefits of Remote Monitoring for Clinical Trials
Who is going to save money, and who is going to pay for remote monitoring? Gonzalez said that sponsors and CROs are going to cut costs with travel, but the time spent reviewing should not change too much.
On the other hand, Sites are going to have to spend a lot of time scanning and uploading paper documents. This process takes time, and a lot of Sites are building it into their budgets, but they need a way to recoup their investment.
One question asked during the session was what’s the approach if you typically do a 100% source data validation but then decide to shift to remote monitoring and only do a percentage of that source data validation? McCarthy said from a risk-based perspective, the key is to document exactly what you are going to do and show that you have control of the risks you’ve identified. Also, it will depend on the timing of your study. If it’s going to end in the next six months or go longer-term giving you a chance to go back later on and perform the additional review.
Do Sites get to choose the solution they use? Or does the sponsor/CRO tell them what they will use? And could we see a standard for how patient medical records come out of an EMR and are bundled, redacted, and placed into a different system, like Agatha?
In Heinz’s situation, they implemented their solution to support their business model, which involved traveling to many locations, not to support remote monitoring specifically. She said that it’s the Site’s responsibility to select the right solution for them. Sometimes there is push-back from the sponsor, but ultimately it’s their choice because they need to do what’s best for them. If the sponsor takes that role and dictates the system to use, it could result in a deviation from standards for the Site, which would be good. She did say that there may be a need to provide direction for new Sites.
The Lightning Round
After the COVID-19 (say 2022), what will be the new reality in terms of remote monitoring? What do we need to do as an industry to ensure it happens.
Gonzalez: We’ll see a hybrid model – 75% remote/25% on-site. In terms of informed consent, we’ll see a lot more eConsent, and the onus will be on the Sites to prove the person who signed the consent really is the person. Also, if there’s a silver lining to COVID-19, it’s that it is forcing countries who don’t allow remote monitoring to rethink their position, because clinical trials are slowing down.
McCarthy: Also agrees it will be a hybrid (60% remote/40% on-site). She said the industry is really in information overload, and they all need to think about what matters. It’s about data, analytics, but also about people, so there needs to be critical thinking that puts the right things into focus.
Heinz: More sites will have adopted some form of eSource or eRegulatory system that enables remote monitoring. They are still doing research and seeing patients, and that needs to continue for the patient and the data. Sites will find a solution of some sort, and they won’t go back. Good technology enhances things, including better ways to measure metrics and quickly get reports that you can’t do in a paper-based world.